This except on menopause, written by Dr Rensburg, bariatric and hormone specialist, gives great insight into the understanding, causes and possible delays in the onset of menopause. Understanding the aging process gives great power through knowledge to change the course of our health and wellbeing.
All information should first be verified by your own doctor before applying any treatment plans or suggestions made below.
Meno-pause (Herapause)
(Ovarian insufficiency and failure)
Menopause (Greek: men- is month) and pause (Greek: pausis) which means the ceasing of the monthly cycles (menses) in women. I do not think the name is quite correct to describe the various stages of menopause, since during the first stage menses usually still occurs and has therefore not ceased (pausis). Climacteric or critical event is also used to describe menopause.
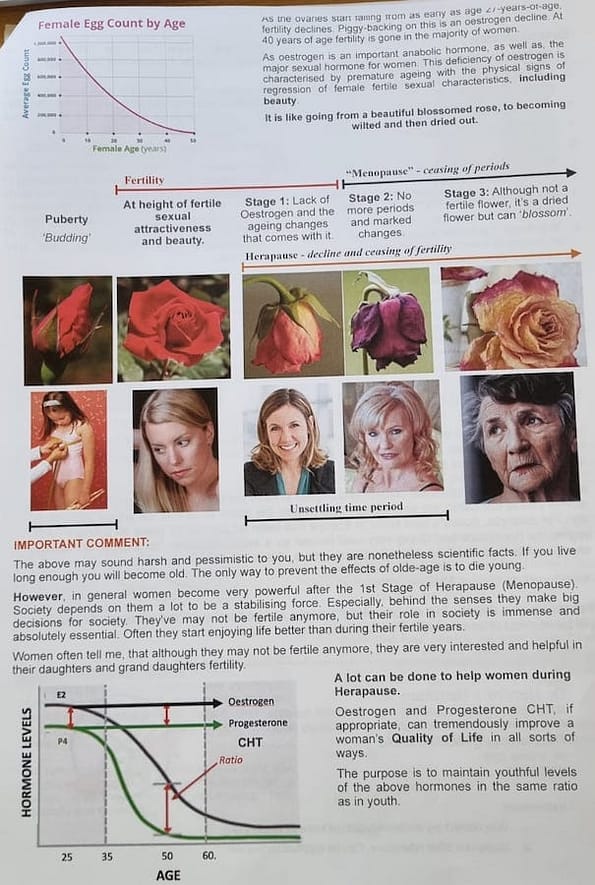
Oestrogen(E2), Progesterone(P4) and fertility decline from the ages 28-33, actually initiating the condition of ‘menopause’.
It is a condition which, at first, causes ovarian insufficiency (with symptoms), followed gradually by ovarian failure (with more severe symptoms). Menopause causes a lack of oestrogen (E2) and progesterone (P4), to the extent that said hormones decrease well below healthy youthful levels.
The consequences of this syndrome, in signs and symptoms, could cause great discomfort for a woman, and may even be debilitating, both physically and emotionally.
There are 3 stages: (Important when it comes to treatment options)
1. From ± 28-33 to about 46 years of age the mentioned hormones decline, leading to ovarian insufficiency, a woman can still fall pregnant, however often needs Progesterone just to hold on to the pregnancy. This is commonly referred to as the peri-menopause. Some symptoms and signs of these declining hormone levels start to manifest itself and gradually worsen.
2. From about 46 to 53 years of age the menses completely ceases, due to ovarian failure and often the symptoms can be quite debilitating. This is what most people understand what ‘menopause’ actually is, but it’s only one phase of it.
3.From around 53 years-of-age onwards a woman gets used to and adapt to the symptoms when she is considered to be in the post-menopause phase. Often women claim at this stage they are “through menopause”.
Fact is you never get “through menopause”. Unfortunately your ovaries won’t make these hormones to youthful levels by themselves again. So, the condition is life long and ongoing and very much part of the ageing process.
What are the symptoms of Menopause?
During the first stage it could be reasonably mild, but gradually gets worse as the situation progresses.
Menopause can be a rollercoaster ride with more downs than ups. Changes include weight gain, changing of your figure, double your chances of heart disease, cause your breasts to sag and moodiness, just to name a few. But this is exactly what Menopause does; it’s a degenerative disease of ageing.
This does not really sound very good – does it? It depends how you look at it. Menopausal women are in a differen prime of their life. Such women play a more powerful role, as mother, as a grandmother and find it easier to compete in the work force, often attaining positions of authority, like a school principle, mentoring, etc. These women can be a real stabilising factor for a family and society. There are other benefits too, in spite of some of the disadvantages of ageing. It could be the start of new opportunities, but a lot of women miss out due to lack of proper treatment as a result of the controversies on the subject.
Should it be treated, or should nature be allowed to take its course?
To treat or not to treat is the question. The prevailing belief is that it should only be treated if there are annoying symptoms, and then only for a short period of time.
Though some women do not experience symptoms, there will always be physical signs and they should be treated. Ultimately, you will have to decide the best course of action once you have looked at the issue from a few different perspective.
How should menopause be treated? The following principles should apply:
1. It should always be preceded by a full medical evaluation. No exceptions. You need the works. This is the time for the big medical of your life and to reflect on the type of life you would like to lead until the end. Your body is not changing for the better
(BTW if you are 50, statistically you have about 260,000 hours left to live. The question is what sort of life you want to lead during this time and even extending it in a healthy way)
2. You should only proceed if you decide it is appropriate for you.
3. The treatment should be comprehensive, not just the toping up of a few hormones, but also attention to your life style, nutrition, and other medical problems, etc. Additionally, you need follow up monitoring and if you do not attend at least once a year for review, you will be deemed off the program and no further prescriptions and treatment will be given.
4. If a treatment plan is proposed, you should use the right tool for the right job. E.g., if your engine oil Is low, do you top it up with olive or canola oil? Menopause is a deficiency of oestrogen PLUS progesterone. That’s what needs to be topped up. Both.
5. But, not just any oestrogen + progesterone. It needs to be biologically equivalent to that which your body actually produces. Premarin is often prescribed in this regard, but is inappropriate since it consists of ‘pregnant mare’s urine’ – made from rejected conjugated equine (horse) oestrogen; It’s not human. (Break one of these tablets up and put it in water – the smell is unmistakeable)
6. It should be given at the levels as produced in the body during youth, say between the age of 20 to 30-year-old and individualised. It shouldn’t be one shoe fits all.
7. Furthermore, CHT should be administered in the same bio-rhythms as in youth. E.g. Oestrogen is a ‘morning hormone’ and progesterone is calming and is an ‘evening hormone’.
8. Additionally, it should not be given every day, because a 25-year-old does not produce the same every day. Thus, the patient should take a break from it for a few days each month in order to mimic the normal youthful bio-rhythms.
9. Although progesterone can be given orally, oestrogen should not be administered orally. Otherwise, it could possibly increase the risk of breast cancer, as well as, suppress your natural somatropin (GH) levels. In the troche form, half is swallowed, and we seldom recommend this delivery system. The transdermal (through the skin) method actually increases somatropin.
10. Since menopause is a deficiency of both oestrogen + progesterone, both should be given, and not alone. They work in tandem. Progesterone can be taken alone for periods of time, but oestrogen correction during menopause will require progesterone as well. (When your engine oil and brake fluid are low, you need to top them both up ‘since the car won’t function well otherwise. Same with progesterone and oestrogen).
11. What about having had a hysterectomy? Some Guidelines state that in such a case only oestrogen should be administered and not progesterone.
However, without a hysterectomy, progesterone must be administered in order to prevent endometrial hyperplasia of the uterus. So, obviously progesterone has a strong controlling influence on oestrogen.

If you study the above, rather mind-boggling illustration, you will notice some lack of logic in determining adding progesterone or not. It’s actually quite simple: the original guidelines developed as a result of the usage of progestins, for example Provera, etc., which are not bio equivalent to human progesterone and have some side effects.
So the logic was:
a. We have no choice to add it to a person still with a womb to prevent endometrial hyperplasia and possible cancer, in spite of some of the side effects like DVT, etc.
b. However, incase of a hysterectomy it is not needed to prevent hyperplasia, and thus to prevent the side effects it is not recommended thus less side effects to deal with. So far so good, but…
What these guideline designers did not take into account was that:
I: Progesterone has many other functions, beyond just preventing hyperplasia. What about sleep effects, bone health, controlling effects on oestrogen, etc.??
II. They did not take into account that we have moved on since, and natural human equivalent progesterone without the side effects of Provera is now on the market. Thus, preserving the good effects of progesterone, without the side effects of Provera. Thus, it can be, and should be, added in the case of hysterectomy.
III. Since we want to preserve, as much as possible, a woman’s normal youthful physiology, it is more physiological that oestrogen and progesterone be used together since they are both deficient in menopause.
IV: Progesterone levels declines much faster than oestrogen and often progesterone CHT becomes necessary before oestrogen is added.
Denying the benefits of progesterone, just because a woman had a hysterectomy is rather strange. Therefore, it should be given after hysterectomy with oestrogen. Besides, these two hormones optimise each-other and progesterone is a vital controller of abnormal effects of oestrogen.
12. When should treatment begin?
Answer: as early as possible when it is necessary. even in the 1st stage of menopause, while still having menses (periods). However, each stage the regime is slightly different to mimic the normal youthful physiology.
13. How long should treatment be?
Due to the breast cancer study (now debunked) in the early 2000’s, doctors became overly cautious. By making the treatment duration short, they hoped there would be less cancer.
You can stop at any time, but you only get the full benefits when you are on it. However, it needs to be evaluated and monitored regularly and decisions made at the appropriate times, rather than arbitrary declare it should only be used for 5 years. (is 5 years and 3 months OK?) New studies come out all the time and ideas change.
14. Difference between HRT and CHT:
In HRT a hormone is replaced by an artificial hormone, for example conjugated horse “oestrogen” in Premarin or the artificial hormones in the contraceptive pill replacing the natural oestrogen and progesterone in such a way that no ovulation takes place. On the other hand, just topping up a natural hormone with a bio-identical equivalent as described before is CHT (Corrective Hormonal Therapy). We believe CHT to be far superior to HRT in the treatment of menopause.
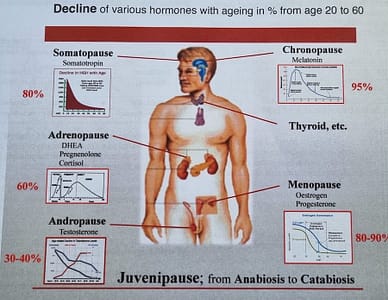
15. Always remember menopause is but a part of Juvenipause,
There are other aspects and hormones that also need to be considered for optimised health.
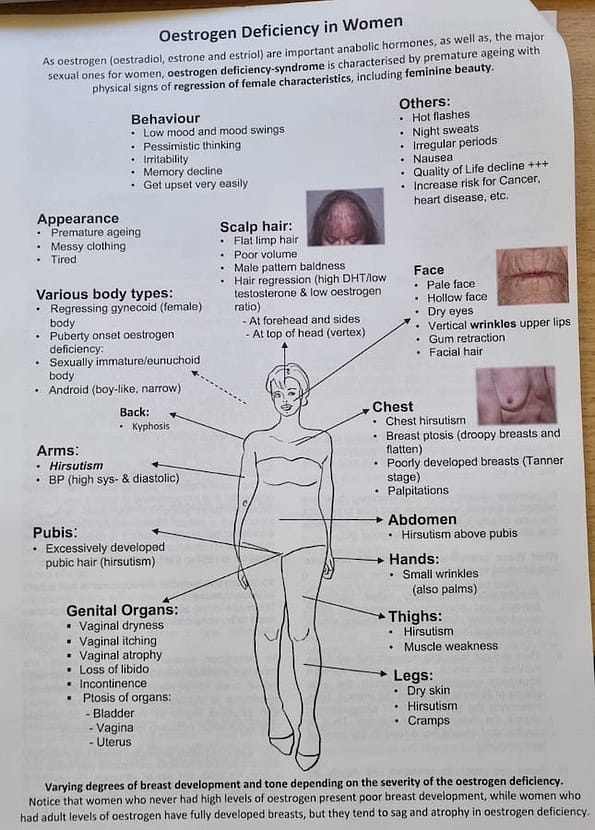
As oestrogen (oestradiol, estrone and estriol) are important anabolic hormones, as well as, the major sexual ones for women, oestrogen deficiency syndrome is characterised by premature ageing with physical signs of regression of female characteristics.
Controversies
- To use hormone therapy in the 1st place (or not?).
- What to use? Phyto-oestrogens, herbs, other lotions and potions, etc.
- How long to use?
- Does it cause cancer, heart disease, dementia?
- What form to use- bio-equivalent or progestins, conjugated equine oestrogen?
- What method of delivery?
- Should progesterone be given, or not, after hysterectomy?
- To just use it every day at some dose, or make an attempt to mimic the physiological rhythms of youthful premenopausal women?
- Its hormones? Isn’t it Bad for you?
- Costs?
It is important that you feel comfortable with all the controversies before you make the decision to participate.
“Menopause” is basically the signalling and eventual end of a woman’s reproductive (fertility) life/cycle. (The pause (interruption) of fertility)
Hera (pronounced ‘Here-a’ not Herra’) was the ancient Greek Goddess of fertility. Hera-pause is a good name to describe “Menopause”. The latter only means the pausing of the menses (periods). The process already starts while women still have periods, thus “Menopause is a misnomer, while Herapause describes in essence what it really is: the process of Fertility pause (Fertility declines and then disappears)
What does this mean to you?
You will be confronted by various doctors, naturopaths and friends about CHT or HRT. There are many views, opinions and personalities out there. You will hear the 10 (and even more) controversies over and over.
It is advised that you study the subject to a degree to have some basic knowledge. Whatever, we advise you at the Clinic, we are willing to do exactly the same to us that we advise patients to do. For example, doctor’s own sister in Europe has been for the last 21 years on a proper CHT regime by her doctor and doing very well indeed as a result. However, as always, knowledge change. Your treatment should be flexible and take all this into account as well.
Any Questions always ASK.
Dr. Hendrik in Rensburg MD
MA. MB Bch. BAO. (TCD) M.R.C.S. (Eng) LR.C.P. (Lond) Faculty Member of the International Hormone Society (IHS)
The Rensburg Medical Clinic +61 8 9444 1766.
AUSTRALIA